Our History
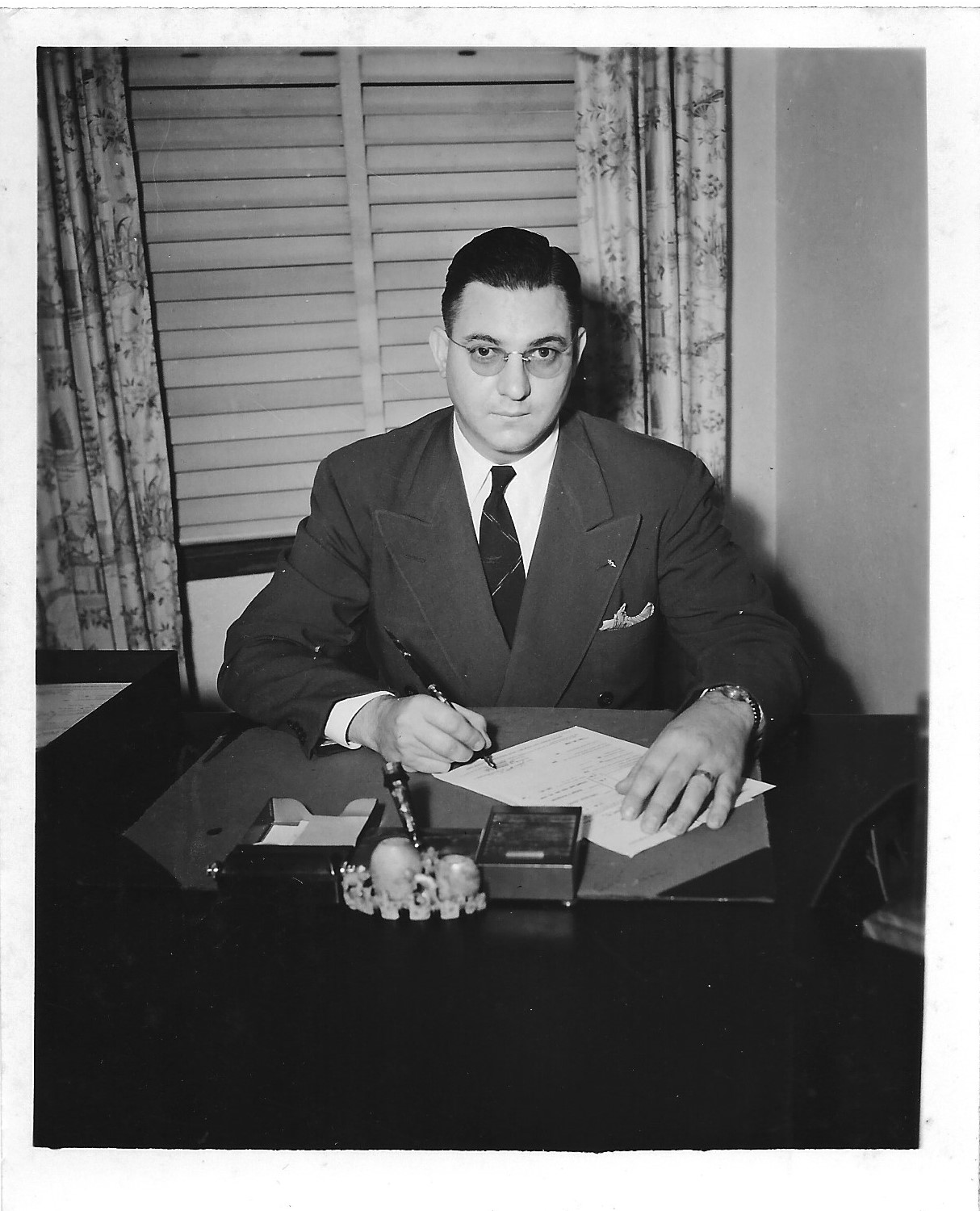
In early 1940, Dr. Forrest J. Pinkerton proposed implementing emergency preparedness measures across Hawaii — including a blood and plasma storage program in the event of an enemy attack.
One of the leading proponents of the measures was Dr. Eric A. Fennel, who is credited with giving Hawaii’s first blood transfusion in 1921 and who operated his own plasma bank out of his home icebox. In December 1940, Dr. Fennel presented his proposal to the Public Health Committee of the Honolulu Chamber of Commerce: a grant to establish a community-wide blood and plasma bank.
Dr. John W. Devereux, Chairman of the Public Health Committee of the Junior Chamber of Commerce, submitted his own proposal, incorporating many of Dr. Fennel’s suggestions. Dr. Devereux’s plan was approved in February 1941 and became the foundation for Hawaii’s first blood and plasma bank.
The Chamber of Commerce established a Civilian Defense Committee consisting of Dr. Pinkerton, Chair; Dr. Nils P. Larsen, Vice Chair; Dr. Fennel; Dr. Devereux; and Dr. F.J. Halford. In addition to assisting with the inauguration of the blood bank, this committee recognized the importance of establishing a disaster training and study center, creating a community blood typing program, and other forms of defense planning for local and national disasters.
The Honolulu Blood Plasma Bank officially opened for donation on June 25, 1941, with Dr. Devereux as manager, Mrs. W.B. Herter as technician, and R. A. Allen Watkins, Mrs. Lucille Watkins, and Walter H. Dillingham as the bank’s first donors. By December 1, the bank had reached its goal: more than 200 flasks of plasma in cold storage in case of emergency.
Just a few days later, on December 7, 1941, Japanese forces attacked Pearl Harbor. In the midst of this disaster, the efforts of the bank proved invaluable. In addition to the stores of lifesaving blood and plasma, more than 700 people lined up to donate at Queen’s Hospital. The Honolulu Blood Plasma Bank went from a maximum of eight donors a day, four days a week, to 50 units per hour, 10 hours a day, every day. Thanks to the foresight of these visionary community leaders, that was only the beginning.
Blood Types
Although all blood is made of the same basic elements, not all blood is alike. In fact, there are four common human blood groups determined by the presence or absence of two chemical markers, or antigens “A” and “B” on the surface of red blood cells. This classification of human blood types is known as the ABO Blood Group System.
Jk3-
This blood, most often found in Polynesians, is some of the rarest in the world. It lacks an antigen that is found on the protein responsible for transporting urea in the red blood cells and kidneys. However, almost 1 out of every 100 Polynesians have Jk3-negative blood. Those who do may only be able to accept Jk3-negative transfusions, so patients at home and around the world depend on us.
A-
About 6% of the population on the mainland has A- type blood. Here in Hawaii, Rh-negative blood types are half as common, with A- making up only 2.6% of Hawaii’s donor population. If you wonder why you should donate blood when there are not so many people with your blood type, remember it only takes one person in need with your blood type to make it the most important.
A+
In Hawaii, A+ is the second most common blood type (32%), so you’re in good company. Sure, lots of people have your blood type but there’s nothing common about your type if it’s not on the shelf when someone needs it.
B-
B- makes up only 0.8% of Hawaii’s donor population. If you’re thinking a small percentage means your donation is, remember it only takes one person in need with your blood type to make it the most important.
B+
B+ is much more common among Asian populations. So it makes sense it’s prevalent in Hawaii making up 16% of Hawaii’s population. More people with your blood type mean your blood type is needed. Even here with lots of B+ donors, sudden high usage of B+ results in unexpected shortages.
O-
As a universal donor, anyone can receive your blood. In an emergency when there’s no time to match the blood type, you save the day. On the mainland, 7-8% of the population has O- blood. Here in Hawaii, you’re in the exclusive 3% club. Your blood type is scarce and patients are always in need of your red blood cells.
As the universal red blood cell donor, you can help everyone, but only O- donors can help you. Which is also why those with O- blood types are always needed! Also, your red blood cells are safest for newborn infants with under-developed immune systems.
O+
O+ is the most common blood type in Hawaii (39%) and is always in high demand. Because your red cells can be given to anyone regardless of the patient’s blood type, your red cells are more impactful than your platelets or plasma.
For O+ donors, the need for your blood changes with the patients’ needs. Depending on the day you come in, you may be asked to donate platelets and/or plasma. When there is no time to find out a person’s blood type, O comes to the rescue. You want as many O+ donors also donating so there is blood on the shelves should you need it. As on O+ donor, you can only receive O type blood.
AB-
Here in Hawaii, Rh-negative blood types are half as common. AB- makes up only 0.4% of our donor population. If you’re thinking a small percentage means your donation is nonessential, remember it only takes one person in need with your blood type to make it the most important.
AB+
In Hawaii, we are lucky to have a higher percentage of AB+ donors. Although it may be small in percentage (6%) it is mighty for patients with uncontrolled bleeding, liver disease, and trauma. As the universal plasma donor, your plasma can be given to anyone regardless of their blood type.
What are MAX Donations?
Blood is made of various components, such as platelets, plasma and red blood cells. A MAX donation gives you the opportunity to make a greater impact by safely and comfortably donating more amounts of just one part of your blood – the part you are uniquely suited to give. Using special donation machines with cutting edge technology, the other components are automatically returned to your body during the donation process.
Find out more about this incredible opportunity and how you can be a part of it by visiting our MAX My Donation page.
How Blood Cells Work
Blood cells fight infection, carry oxygen and help control bleeding. They are produced in bone marrow, especially the vertebrae, ribs, hips, skull and sternum. Among other components, blood cells consist of red cells, white cells, platelets and plasma
Red cells deliver oxygen.
Red cells are disc-shaped cells containing hemoglobin, which enables the cells to pick up and deliver oxygen to all parts of the body.
White cells defend the body.
White cells are the body’s primary defense against infection. They can move out of the blood stream and reach tissues being invaded.
Platelets help control bleeding.
Platelets are small fragments of cells in the blood that control bleeding. They form clusters to plug small holes in blood vessels and assist in the clotting process.
Plasma carries blood cells.
Plasma is a pale yellow mixture of water, proteins and salts. One of the functions of plasma is to act as a carrier for blood cells, nutrients, enzymes, hormones and proteins including clotting factors.
Donor Safety is Our Top Priority
Donors are given a mini physical, which includes checking blood pressure, pulse and temperature. In addition, a hemoglobin level is performed before the donation to make sure donors have enough blood to safely give away one pint. A trained nursing team member is present at all times.
All equipment used for the blood donation is sterile and disposable, used only once. It is impossible to get HIV/AIDS or hepatitis by giving blood.
Our goal every day: 100% safe blood.
The blood supply in the United States is much safer today than ever before. The risk of HIV transmission via blood has been nearly eliminated and the risk of hepatitis transmission greatly reduced thanks to multiple levels of safeguards, including:
- Comprehensive evaluation of donors’ medical history to exclude donors who may be carriers of infectious agents
- Physical examination of the donor
- Strict donation procedures using sterile supplies
- Laboratory testing
These procedures are followed by all blood centers nationwide and are monitored under the regulatory guidance of the Food and Drug Administration (FDA).
Only volunteers are permitted to donate blood, and there are no incentives to give.
Studies prove that community volunteers are the safest source of blood for transfusion. Every donor completes a health history questionnaire and screening interview to identify donors who may be at risk for carrying blood-borne diseases. Strict confidentiality, as well as the absence of incentives or pressure to donate, encourage honest answers, and deferral of any potential donor with possible health risks.
Donated blood is tested for evidence of infectious disease, including hepatitis B and C, HIV 1 and 2, HTLV I and II, syphilis, West Nile virus and Chagas disease. The donor’s blood type is also determined. Any unit of blood that shows evidence of carrying an infectious disease is discarded and the donor is notified and deferred from subsequent donations until free of infectious disease, although some deferrals may be permanent.